参考文献
[1]Korkama E-S et al. EHA Learning Center. Kjellander C. 2018;214791; PF314.
[2]Morado M et al. Clin Cytom. 2017;92:361-370.
[3]PNH Registry (2013) PNH National Service- Leeds and London
[4]Hill A, et al. Paroxysmal nocturnal haemoglobinuria. Nat Rev Dis Primers 2017;3:17028.
[5]Risitano AM and Rotoli B. Paroxysmal nocturnal hemoglobinuria: pathophysiology, natural history and treatment options in the era of biological agents. Biologics 2008;2(2):205–222.
[6]Risitano AM. Paroxysmal nocturnal hemoglobinuria and the complement system: recent insights and novel anticomplement strategies. Adv Exp Med Biol. 2013;735:155–72.
[7]Hill A, et al. Eculizumab prevents intravascular hemolysis in patients with paroxysmal nocturnal hemoglobinuria and unmasks low-level extravascular hemolysis occurring through C3 opsonization. Haematologica 2010;95(4):567–573.
[8]Risitano AM. Anti-Complement Treatment in Paroxysmal Nocturnal Hemoglobinuria: Where we Stand and Where we are Going. Transl Med UniSa. 2014;8:43–52.
[9]Debureaux P, et al. Hematological Response to Eculizumab in Paroxysmal Nocturnal Hemoglobinuria: Application of a Novel Classification to Identify Unmet Clinical Needs and Future Clinical Goals. Blood. 2019;134(Suppl 1):3517.
[10]Jang JH, et al. Iptacopan Effectively Controls Intra- And Extravascular Hemolysis And Leads To Durable Hemoglobin Increase In Patients With Treatment-Naïve PNH. Abstract presented at the 26th Annual Congress of the European Hematology Association (EHA) 2021.
[11]Schubart A, Anderson K, Mainolfi N, et al. Small-molecule factor B inhibitor for the treatment of complement-mediated diseases. Proc Natl Acad Sci U S A. 2019;116(16):7926-7931. doi:10.1073/pnas.1820892116.
[12]Novartis. Data on file.
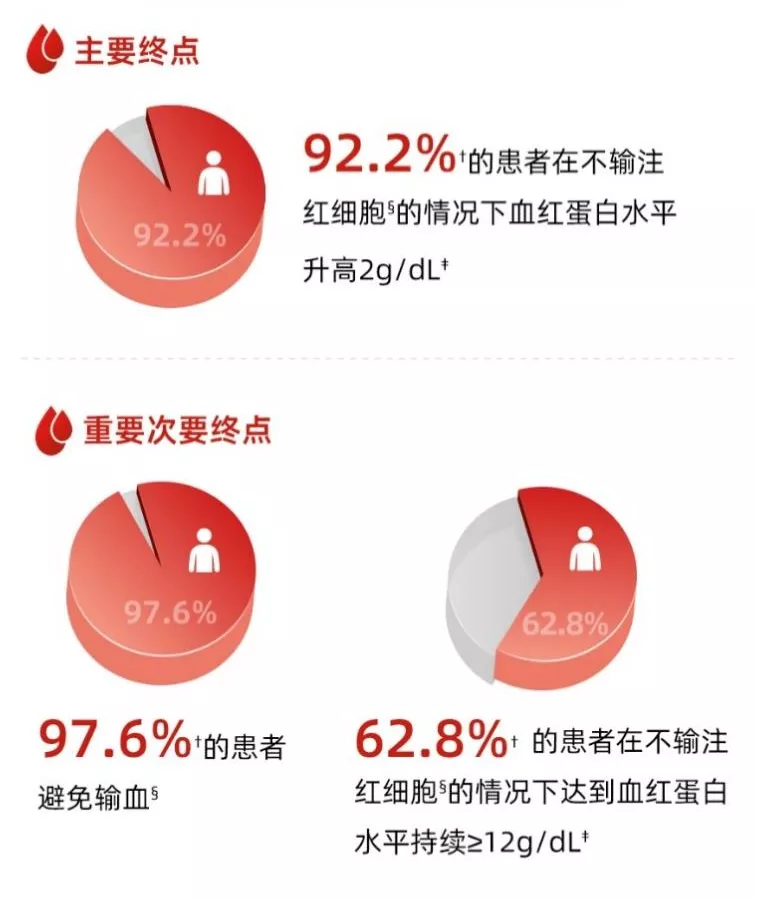
[13]A.M. Risitano, et al. Oral complement factor B inhibitor iptacopan monotherapy improves hemoglobin to normal/near-normal levels in paroxysmal nocturnal hemoglobinuria patients naÏve to complement inhibitors: Phase III APPOINT-PNH trial. OS12-06; 2023 EBMT.
[14]Available at https://www.cde.org.cn/main/xxgk/listpage/da6efd086c099b7fc949121166f01…. Accessed April 2023.
[15]Clinicaltrials.gov. Study of Efficacy and Safety of Iptacopan in Patients With C3 Glomerulopathy. (APPEAR-C3G). Available at https://clinicaltrials.gov/ct2/show/NCT04817618. Accessed September 2022.
[16]Clinicaltrials.gov. Study of Efficacy and Safety of LNP023 in Primary IgA Nephropathy Patients (APPLAUSE-IgAN). Available at https://clinicaltrials.gov/ct2/show/NCT04578834. Accessed September 2022.
[17]Clinicaltrials.gov. Efficacy and Safety of Iptacopan (LNP023) in Adult Patients With Atypical Hemolytic Uremic Syndrome Naive to Complement Inhibitor Therapy (APPELHUS). Available at https://clinicaltrials.gov/ct2/show/NCT04889430. Accessed September 2022.